In labor, the mother and baby are tested to their limits. It’s a high-stakes event, and the baby might not respond well to the pressure. When that happens, it’s called fetal intolerance to labor.
In this article, we’ll explore why fetal intolerance of labor happens. We’ll also discuss what doctors can do to help a baby through this challenging phase as safely as possible.

What is Fetal Intolerance to Labor?
Fetal intolerance to labor is when the fetus can’t handle the stress of labor. Usually, it’s because oxygen supply has been reduced, or some other complication is affecting the baby. It can make the baby’s heart beat faster, slower, or in irregular patterns.
Here are the key indicators of fetal intolerance of labor:
- Abnormal fetal heart rate patterns: These can show up as either too high or too low heart rates or other irregularities.
- Reduced fetal movement: The baby may move less than usual, signaling distress.
- Signs of acidosis: The fetus may develop a condition called metabolic acidosis, which is an excess of acid in the blood due to inadequate oxygen.
Fetal Distress vs. Fetal Intolerance to Labor
Fetal distress and fetal intolerance of labor are related terms. You might see (or hear) them used interchangeably.
Both terms refer to situations where the fetus isn’t coping well with the stress of labor. But they’re used in slightly different contexts.
- “Fetal distress” refers to any situation where the fetus shows signs of not getting enough oxygen or experiencing other complications. It can happen any time during labor and delivery.
- “Fetal intolerance to labor” is a more specific term. It refers to a situation where the fetus is struggling to handle the physiological stress of labor itself.
In other words, fetal intolerance to labor is a type of fetal distress. This term focuses specifically on how the baby responds to the stresses of labor.
What Causes Fetal Intolerance to Labor?
There’s a lot going on during labor! It’s like the final hurdle in a race—one last challenge for the baby to endure before entering the world.
During labor, the baby has to weather a storm of physiological changes, including:
- Slightly reduced oxygen supply
- Increased pressure
- Blood flow changes
These major changes during labor can just become “too much” for a baby. Some babies have trouble adapting to them.
Plus, there are factors that can make labor even more stressful for a baby. They include:
- Umbilical Cord Compression: The cord becomes compressed, or “squished”, restricting blood flow and oxygen to the baby.
- Placental Insufficiency: The placenta isn’t delivering enough oxygen and nutrients.
- Maternal Health Conditions: Conditions like high blood pressure, diabetes, or preeclampsia can impact how well the baby handles labor.
- Abnormal Uterine Contractions: Contractions that are too strong or too frequent can overwhelm the baby and limit the oxygen supply.
How Can Doctors Help a Baby Under Distress?
When a baby shows signs of fetal intolerance to labor, doctors have several strategies to ensure a safe delivery:
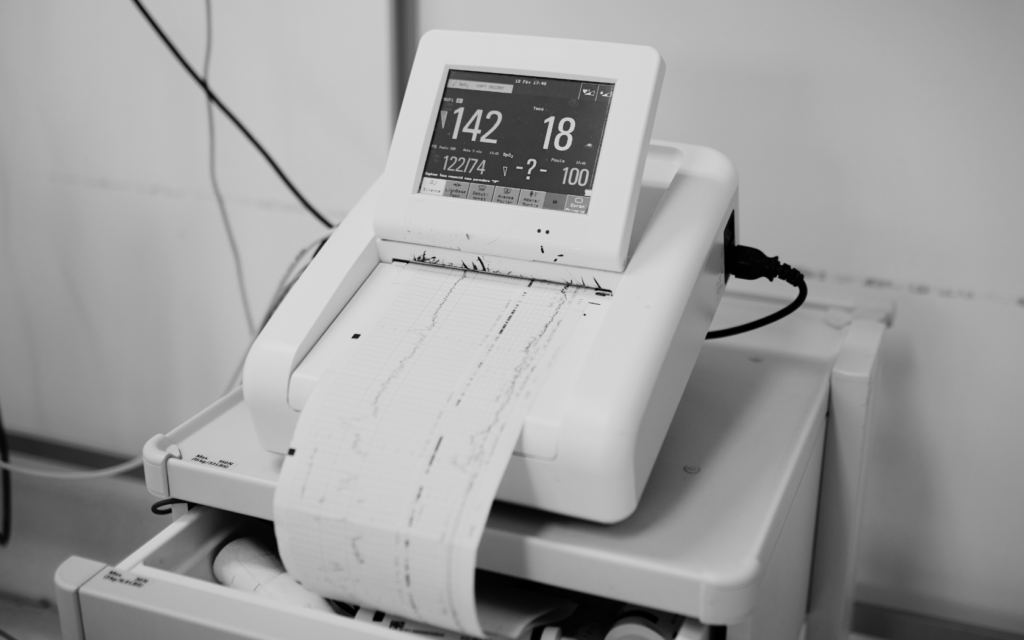
Monitor the Heartbeat
Doctors track the baby’s heartbeat. They look for distress signals and try to understand how severe the situation is before deciding on the best course of action.
Manage Contractions
Sometimes contractions are too strong and frequent. That can cause fetal intolerance of labor. Doctors might adjust medications or interventions to ease the stress on the baby. They might give the mother medication to slow down contractions.
Improve Oxygen Supply
Doctors might reposition the mother while she’s in labor. This could enhance blood flow and help the baby get more oxygen. They might administer oxygen to the mother as well.
Amnioinfusion
Doctors might add fluid to the amniotic sac. This can relieve umbilical cord compression and improve cushioning.
Manage Maternal Conditions
A mother’s health conditions can affect a baby’s health throughout pregnancy, and during labor, too! It’s important to keep conditions like high blood pressure and diabetes under control. This will minimize their impact on the baby during pregnancy and labor.
Emergency C-Section
If intolerance to labor becomes severe, the baby needs to be delivered right away. Doctors can order an emergency cesarean section. Then they can administer medical treatment to the baby if needed.

What If a Doctor Doesn’t Address Fetal Intolerance of Labor?
If a doctor doesn’t address the baby’s intolerance, it can lead to serious complications, such as:
- Brain damage from lack of oxygen
- Birth injuries, like fractures or nerve damage
- Acidosis (too much acid in the blood, which can affect the organs)
- Stillbirth
- Severe bleeding or infection in the mother
If your doctor failed to act when your baby was in distress, and your baby was injured, you may have grounds for a medical malpractice lawsuit. Contact our experienced lawyers to find out if you have a case.
Fetal Intolerance to Labor FAQs
Fetal distress during labor occurs in about 10% to 25% of pregnancies. This broad range is due to varying definitions and cases where the fetus may not be receiving enough oxygen. The estimates also differ because “fetal distress” is not consistently defined across medical sources.
Most cases of fetal distress are managed without major complications. Doctors monitor the fetal heart rate to detect abnormalities early. That way, they can intervene if needed. They might provide oxygen, change the mother’s position, or perform an emergency C-section.
The signs of fetal intolerance to labor include:
– Not moving much in the womb
– Very low heart rate (bradycardia)
– Irregular heart rate (arrhythmia)
– Very high heart rate (tachycardia)
– Meconium (the baby’s first stool) in the amniotic fluid
Signs of fetal distress include a decrease in baby movement, abnormal heart rate, and cramping or pain. Vaginal bleeding or unusual fluid leakage can also be a warning sign. Contractions that are too frequent may reduce oxygen to the baby. If any of these occur, call your doctor right away.
If your baby isn’t moving as usual, you might do a “kick count”. Lie down on your side. Set a timer, and see how long it takes for the baby to make 10 movements. The American Congress of Obstetricians and Gynecologists (ACOG) says it’s ideal to feel at least 10 movements in 2 hours.
Babies often have quiet periods. So, according to the ACOG, sometimes it’s ok not to feel 10 movements in 2 hours. But a significant reduction in movement can be a concern. If you feel your baby is moving less or the movements are weak, call your doctor. It’s always better to check with a doctor than to wait too long.




